About a year ago I adopted a mainly plant-based diet, or as my colleagues jokingly call it, a flexitarian which is a term to describe a vegetarian who very rarely eats meat.
To preface my decision to radically change my diet, it helps to have a bit of a background. In October of 2015 my Mom was diagnosed with Primary Progressive Multiple Sclerosis, and at the time there were no medications to prevent or reverse disease progression. In Spring of 2016 my mom had a relapse and took a pretty serious fall and ended up fracturing her eye socket and nose. (to read more about my mom’s diagnosis, check out my Breaking Bad News blog post). Frustrated that there were no pharmacologic treatment options, we began looking elsewhere for symptom management. This is when we discovered Dr. Terry Wahls.
Dr. Wahls is an internal medicine doctor who was diagnosed with relapsing remitting  multiple sclerosis which eventually became so severe she was wheelchair bound. Using her medical background she researched which vitamins and supplements were good for brain and nervous system health. This lead her to develop the Wahls Protocol which is a modified version of the Paleo diet. This diet focused on limiting dairy products, eggs, added sugars and increasing the intake of leafy green vegetables, brightly colored fruits, healthy fats, and high quality meats and fish.
multiple sclerosis which eventually became so severe she was wheelchair bound. Using her medical background she researched which vitamins and supplements were good for brain and nervous system health. This lead her to develop the Wahls Protocol which is a modified version of the Paleo diet. This diet focused on limiting dairy products, eggs, added sugars and increasing the intake of leafy green vegetables, brightly colored fruits, healthy fats, and high quality meats and fish.
When we first attempted to follow the Wahls Protocol, it felt impossible to incorporate 9 cups of fruits and veggies daily like Dr. Wahls recommended. Gradually over time my family transitioned our diet from the Wahls diet, to a mostly vegetarian diet. This was a huge jump from the meat-and-potatoes style meals I had grown up eating. My family’s decision was further reinforced by some of the excellent food documentaries available on Netflix and Amazon Video (which I will link below). What started out as an experiment to reduce my mom’s multiple sclerosis symptoms became a lifestyle when we all began to feel better. My cholesterol levels improved drastically, I lost 10 lbs, my skin improved and I never felt bloated on experienced heart burn after a large meal.
Fast forward a couple of months I was eating a diet that was 75-80% vegetarian with an occasional cheat meal. Everything was going well until I started my outpatient family medicine rotation. I had just completed my trauma surgery audition, where I was working 13 to 14 hour shifts 6 days a week, and now I was being spoiled with my 9 am to 3pm schedule with an hour lunch break to boot. Despite working far less hours and enjoying my free nights and weekends, I felt terrible. I’d drive home over my lunch break and feel myself straining to keep my eyes open during my 5 minute drive. I would nap over my lunch and chug coffee during my afternoon appointments yet I would still feel drained at the end of the day. I scheduled an appointment with a new primary care physician (PCP) to discuss my new onset fatigue. I mentioned in passing that I had drastically cut back on the amount of meat and animal products and I was instantly interrupted. My PCP was entirely convinced my fatigue was due to my new “alternative diet” as he called it.
I shook my head, sure that that was not the issue. Not wanting to overstep my bounds as a patient, but not wanting to leave the appointment without a diagnosis I asked if I could have some blood work done. My PCP reluctantly agreed and the results indicated that I had an acute mononucleosis infection. Mononucleosis, also known as Mono or the “Kissing Disease” is a virus spread via saliva which can be transmitted between people via coughing, sneezing, sharing utensils or drinks, or kissing an infected person. While mono can cause a variety of symptoms including fever, sore throat, enlarged lymph nodes, the predominant symptom is fatigue that lasts for several weeks to months. Despite blood work clearly indicating mono was the culprit, my PCP lectured me on eating a “well balanced diet”. He encouraged me to incorporate meat back into my diet to assure I was getting all the nutrients my body needed.
While I do believe this doctor had good intentions when he suggested dietary changes, I do not believe he had the appropriate education to make said suggestions.
In 1985, the National Academy of Sciences conducted a study to determine how much nutrition education medical students received. At the time of the study only 27% of the responding schools had a dedicated nutritional course. The study concluded by stating that “nutrition education programs in US medical schools are largely inadequate to meet he present and future demands of the medical profession”. Although that study was done more than 30 years ago, it’s estimated that that now only 1/5 of medical schools have a nutrition course, and most medical schools teach less than a total of 25 hours of nutrition over the course of four years.
During my entire medical school career I have had one lecture on nutrition and one meeting with a nutritionist. Over the past 4 years I have had less than 4 hours of nutrition education, yet when I work in an outpatient setting I am asked at least once a day for dietary recommendations. When a patient asks me for dietary recommendations most of what I discuss with them is information I have acquired due to my interest in nutrition, health and well being and not because of my pursuit to become a doctor.
What a scary thought!
I think as a (soon-to-be) physician I often underestimate the type of influence I can have on my patients. While I believed I am well educated in nutrition, I have no formal training and no qualifications to be suggesting any sort of diet to a patient. Although I have found success in following a plant-based diet, I don’t believe it is appropriate to suggest this a solution to all of my patients. Furthermore I would feel completely unprepared to discuss a Diabetic Diet, the Dash Diet, a Keto diet, or any other diet frequently recommended to patients by a specialty doctor. Yet doctors are frequently the only healthcare provider that patients will contact to get advice on diets. Not only are we ill prepared to discuss diets we also often lack the time to education and advise patients on food, meal plans, or dietary resources.
 What’s even more frustrating is we know there is connection between poor diet and preventable disease. In fact the father of modern medicine himself, Hippocrates, was quoted as saying “Let thy food by thy medicine and thy medicine be thy food” and for thousands of years plants and herbs did serve as the only medicine we had to treat any medical condition.
What’s even more frustrating is we know there is connection between poor diet and preventable disease. In fact the father of modern medicine himself, Hippocrates, was quoted as saying “Let thy food by thy medicine and thy medicine be thy food” and for thousands of years plants and herbs did serve as the only medicine we had to treat any medical condition.
One of the biggest implications of a poor diet is the prevalence of obesity in the United States. According to the CDC 70.7% of US adults 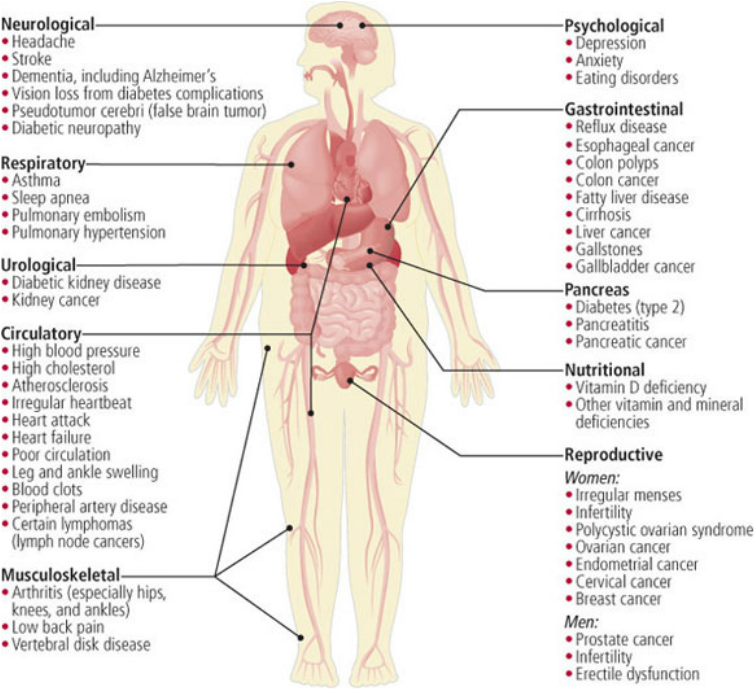 (over the age of 20) are overweight or obese. It is well established that being overweight increases a patient’s risk of more than 50 different health concerns including depression, sleep apnea, heart disease, and colon cancer (see image to the right) Weight gain is due to consumption of more calories than are expended and any diet that limits the number of calories consumed should result in weight loss. As a healthcare provider doctors should be equipped in being able to counsel a patient on weight loss, but sadly we are not provided those tools during our 4 years of medical school.
(over the age of 20) are overweight or obese. It is well established that being overweight increases a patient’s risk of more than 50 different health concerns including depression, sleep apnea, heart disease, and colon cancer (see image to the right) Weight gain is due to consumption of more calories than are expended and any diet that limits the number of calories consumed should result in weight loss. As a healthcare provider doctors should be equipped in being able to counsel a patient on weight loss, but sadly we are not provided those tools during our 4 years of medical school.
One of the major potential side effects of obesity is diabetes. A 2015 study found that more than 30 million Americans have diabetes, which equates to 9.4% of the population and it is estimated that 84.1 million Americans are prediabetic. The medical costs and money lost due to reduced productivity as a direct result of diabetes is estimated at $245 billion per year. Diabetic nephropathy accounts for 45% of End Stage Kidney Disease cases. The complications of diabetic neuropathies account for 67% of limb amputations in the United States and diabetic retinopathy is the leading cause of blindness in American adults. Furthermore, diabetes now accounts as the 7th leading cause of death in the United States.
As a medical student, I have never had the opportunity to discuss a diabetic patient’s diet with them when they come to clinic for a follow up appointment. Typically when a patient has a chronically elevated A1c and too high fasting or postprandial blood sugar levels, we adjust the dose of their insulin or consider changing the type of diabetic medication they are on. Frustrating doesn’t even begin to describe the feeling of chasing symptom control, when there is a blatantly obvious solution to the problem available to our patients: diet.
There is well documented evidence to prove that a high fiber, low fat vegetarian diet can have drastic results on the management of diabetes. To quote this article that appeared in the Journal of Education and Health Promotion regarding the prevention and control of type-2 diabetes, “The vegan diet is based on American Diabetes Association (ADA) guidelines; the results of this study were astounding: Forty-three percent of the vegan group reduced their diabetes medications. Among those participants who didn’t change their lipid-lowering medications, the vegan group also had more substantial decreases in their total and LDL cholesterol levels.” There is also a very brief article regarding the vegetarian diet on the American Diabetes Association’s webpage as well as a link to purchase the “American Diabetes Association Vegetarian Cookbook” which has been available of the ADA’s website since 2014.
Despite evidence of the benefits of following a plant based diet in 2014, it wasn’t until the 2018 Standards of Medical Care in Diabetes was released that the ADA was fully in support of recommending a plant based diet. This decision was based on a comprehensive report cites 35 studies pointing to the benefits of a plant-based diet, and also notes that doctors and nutritionists should “always” include “education on lifestyle management.”
Now is the time we need to start changing the way we practice medicine. Instead of focusing on treating symptoms and battling chronic conditions we should redirect our aim at preventing disease. Since medical schools have not yet equipped us with the ability to prescribe diet as easily as we can prescribe medications, it is up to us to educate ourselves and to be a advocate for our patient’s health. I believe that nutritionists should play a much larger role in a the treatment plan of patients and that medical facilities should make an effort to provide patients with resources on diet and nutrition.

If you’ve been following my blog for a while, you may have seen my blog post about the sustainability of meat consumption. If you didn’t see it and are curious to learn about the environmental cost of eating meat, check out my post on the Hidden Cost of a Hamburger
And lastly, as promised here is my very long list of books and documentaries about the food industry and the effects on diet and health.
Books
Documentaries
What The Health (Netflix)
Food, Inc (Netflix)
Food Choices (Netflix)
In Defense of Food (Netflix)
Forks Over Knives (Netflix)
Hungry for Change (Netflix)
Cowspiracy (Netflix)
Fed Up (Netflix)
Fat, Sick and Nearly Dead (Netflix and Amazon)
The Okinaway of Life (Amazon)
Supersize Me (Amazon)
Food Matters (Amazon)
A River of Waste (Amazon)
A Meaty Issue: Thinking Beyond Your Dinner Plate (Amazon)
At the Fork (Amazon)
Meat (Amazon)
Vegan: Everyday Stories (Amazon)
I absolutely agree! Doctors need to have a Registered Dietitian on their team/ in their facility. While doctors are most often asked about diets, we need an integrated team approach where doctors can refer to the nutrition experts.
LikeLike